
Can a one-star skilled nursing facility be the same as a five-star facility? It depends on your zip code.
When the Centers for Medicare & Medicaid Services assigns the health inspection rating domain, which drives the overall star rating calculation, it stratifies performance within each state before giving one to five stars based on percentiles.
Who knew CMS grades SNFs on a curve? It seems fair enough given the nuances across state and regional survey offices, right? Wrong.
Consider the two skilled nursing facilities below that have equivalent staffing levels, resident acuity and quality measure performance:
- Facility A is 175 beds, located in Washington and received 11 citations over the past three survey cycles.
- Facility B is 175 beds, located in New Hampshire and received the same 11 citations during the same timeframe as Facility A.
Based on CMS’s April 2021 Care Compare data, Facility A is rated five stars for health inspections, while Facility B is rated only one star. Facility A qualifies for the best financing and favorable loan covenants because it has no Special Focus Facility risk, a higher overall star rating and optimal marketing.
While Facility B is not at risk for being an SFF and has the same survey outcomes, it may not get the best financing. Because of its one-star health inspection rating, its overall rating cannot be upgraded by more than one star based on staffing and quality measures. That limits Facility B to a maximum rating of two stars overall, even if it has five-star performance for both staffing and quality measures like Facility A.
How can that be? Why do two facilities with identical survey outcomes have different star ratings that lead to different financing and marketing opportunities?
The following chart shows the health inspection scores that currently qualify for five-star health inspection ratings per state:
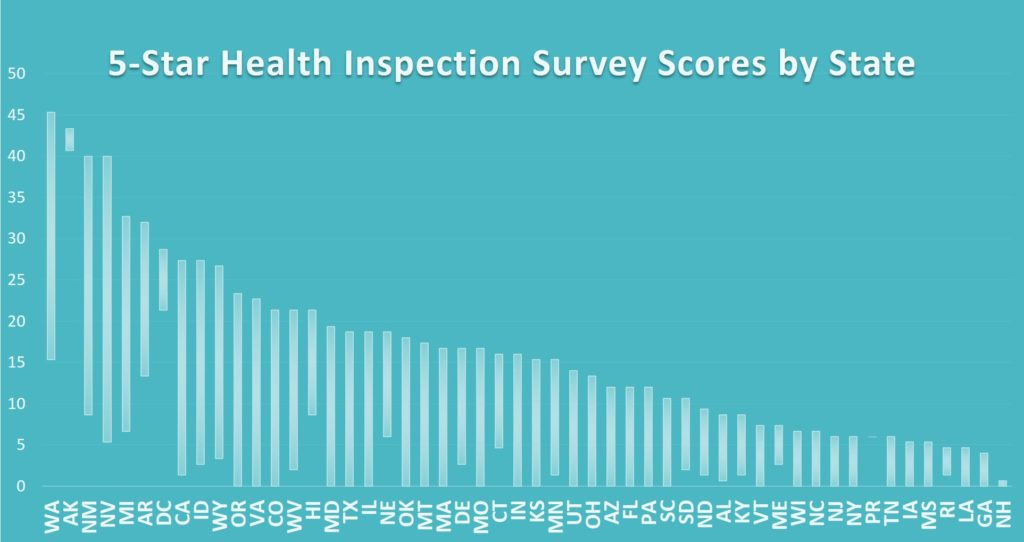
Higher health inspection survey scores indicate more citations, more severe citations, more recent citations, and/or difficulty getting back into compliance. In states to the right side on the above chart, very low health inspection score thresholds qualified for health inspection ratings of five stars, indicating few citations, less severe citations, and a quick return to compliance when deficiencies were cited. But for states on the left side, higher scores (worse health inspection performance) still qualified for health inspection ratings of five stars, making it “easier” to obtain a higher rating in those states.
A facility rated only one star for health inspections in New Hampshire, Alabama, Maine, New Jersey, Georgia, New York, Tennessee or North Dakota could qualify for a five-star rating in Washington, Alaska, Michigan, New Mexico, Nevada or Arkansas based on geography alone with no change in performance.
While this state stratification methodology may give a relative performance indicator to local consumers, it can skew the understanding of facility performance and impact not only star ratings but other important factors like financing, insurance premiums, marketing, staff morale, special focus candidacy, litigation, negative press and more.
An overall rating of one or two stars and/or SFF candidacy is a big deal to lenders, including HUD, and a big red flag in marketing. The table below shows the SFF candidate survey scores in each state:
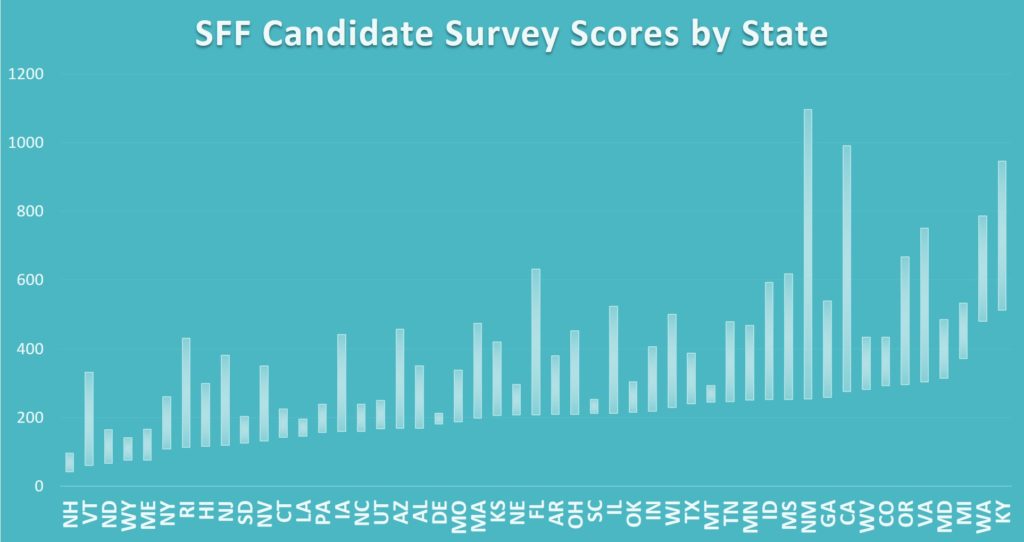
As you can see, all SFF candidates are not created equal. Facility A located in Washington with a survey score of 42 is awarded a five-star rating for health inspections but would qualify as an SFF candidate and a one-star health rating if relocated to New Hampshire.
Understanding your facility’s data and your peers’ data is key, so you can accurately present and defend facility performance in marketing, financing efforts and more. If the states where you operate suddenly shift to fewer survey citations, facilities could be negatively impacted with drastic rating declines even while maintaining superior performance.
We know that state survey offices cite unequal quantities of deficiencies, so it’s not a bad idea to use the state stratification method to ensure facilities are not unjustly penalized, and variation is accounted for by “grading on a curve.”
However, perhaps the industry should advocate for CMS to establish baseline maximum score criteria for the health inspection ratings that would allow more facilities in low score states to achieve three-, four-, and five-star ratings, while incentivizing facilities in all states to improve rather than forcing them down to lower star levels and unfairly impacting their marketing efforts, financing abilities, and more.
Jessica Curtis, CHFP, CRCA is a Managing Director at Formation Healthcare.





