
Telehealth Awareness Week (September 19–25) is a time to highlight and reinforce the critical role of telehealth.
Telehealth is the use of telecommunications technology to deliver care and health services remotely, and it plays an increasingly important role in our healthcare ecosystem. I’d like to take this opportunity to reflect on five simple yet significant observations regarding virtual care in skilled nursing facilities.
1. Telehealth has been legitimized
Although telehealth has been around for decades in the United States, insurers (including the Centers for Medicare & Medicaid Services) were unwilling to reimburse for telehealth-based care, which hampered its wide-scale adoption. That all changed with the onset of the COVID-19 pandemic.
Facing a situation where people without COVID-19 couldn’t access normal care, federal lawmakers in March 2020 eased the rules on telehealth access and coverage (including the rules for skilled nursing facilities) and passed a $500 million spending plan to expand telehealth services as an alternative to in-person hospital visits. In doing so, Congress “let the genie out of the payer bottle” by legitimizing telehealth as a reimbursable modality of care.
2. SNFs are receptive to telehealth
In response to the aforementioned federal actions, evidence suggests SNFs have widely embraced telehealth. One study, for example, reported an 11-fold increase in SNFs’ use of telehealth between March and August 2020.
We don’t know what percentage of SNFs leverage telehealth services or whether they’ve kept using those services after the initial rush, so I won’t speculate on SNFs’ current receptiveness to telehealth. But using the number of established and niche telehealth vendors offering SNF-specific solutions as a barometer of market demand, it is safe to say that, at a minimum, a notable segment of SNFs are very receptive to incorporating telehealth into their care delivery model.
3. Broadband access is not a barrier to telehealth for most SNFs
For telehealth to be feasible, devices should be able to connect to the internet at broadband speeds (defined as a download speed of at least 25 megabytes per second). With approximately 120.4 million people in the United States (36% of the population) not using the internet at broadband speeds and 14.5 million U.S. residents (4%) having no access to broadband at all, I was curious how these measures looked when applied to SNFs.
To help replicate this research, I reached out to Lorren Pettit of GeroTrend Research, an advisor to the American Telemedicine Association (ATA) and collaborator with ZHSG on various Five-Star improvement projects. Employing Microsoft’s December 2020 United States Broadband Usage Percentages Dataset to partition ZIP codes into 11 “broadband usage ranges,” we discovered that only 40 (0.3%) U.S. SNFs in the Aug. 1, 2021, Nursing Home Compare database operate in a ZIP code projected to have no broadband access at all (Figure 1). This is a hopeful finding.
4. SNF broadband usage might dampen telehealth adoption
To estimate the number of SNFs not accessing the internet at broadband speeds, we calculated the average broadband usage in each of the 11 broadband usage ranges, and then multiplied by the number of SNFs operating in each range. This yielded a total of 9,095 SNFs estimated to be using the internet at broadband speeds (Figure 1). With just over 15,000 SNFs in the United States, that leaves roughly 6,000 SNFs (40% of U.S. SNFs) estimated to not access the internet at broadband speeds, though broadband is mostly available across the country.
Commenting on these findings, Ann Mond Johnson, the ATA’s CEO, noted the importance of closing the “digital divide” in underserved and rural patient populations, “including the nation’s nursing homes where the experiences of the pandemic uncovered significant vulnerabilities.”
I am not one to ring the alarm bell prematurely; in fact, I strongly suggest this issue needs further study. But if this finding can at least be considered directionally correct, then it is concerning. It suggests broadband usage, rather than broadband access, may be a limiting factor for the widespread advancement of telehealth in SNFs.
| Broadband Usage Range | Avg. Broadband Usage | # of SNFs | % of SNFs | Est. # of SNFs Using Broadband Speeds |
| 100% | 100.0% | 2,494 | 16.4% | 2,494 |
| >=90% <100% | 94.8% | 1,025 | 6.8% | 972 |
| >=80% <90% | 84.9% | 1,304 | 8.6% | 1,108 |
| >=70% <80% | 75.0% | 1,306 | 8.6% | 979 |
| >=60% <70% | 64.8% | 1,505 | 9.9% | 976 |
| >=50% <60% | 54.9% | 1,519 | 10.0% | 834 |
| >=40% <50% | 44.9% | 1,543 | 10.2% | 692 |
| >=30% <40% | 35.0% | 1,430 | 9.4% | 501 |
| >=20% <30% | 25.1% | 1,331 | 8.8% | 334 |
| >=10% <20% | 15.1% | 1,113 | 7.3% | 169 |
| >0% <10% | 6.5% | 555 | 3.7% | 36 |
| 0% | 0.0% | 40 | 0.3% | 0 |
| 15,165 | 9,095 |
5. Telehealth could improve Five-Star QMs
Of the array of quality measures used to calculate a SNF’s Five-Star rating, a few measures (e.g., outpatient emergency department visitations; the use of antipsychotic medications) stand out as ripe for improvement through using virtual care interventions to connect with physicians/specialists.
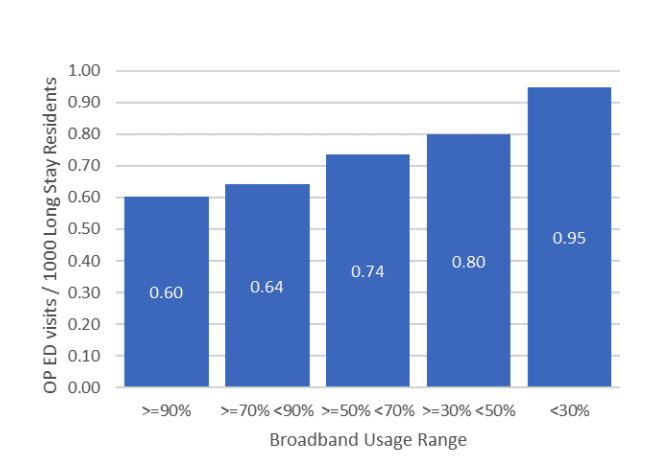
Early evidence supports this idea. Researchers at the University of California in Irvine, for example, found that when six SNFs used a telehealth platform, they reduced unnecessary transfers by as much as 80%. Even our own analysis of SNF performance by their projected broadband usage supports this study. We found a compelling association between a SNF’s projected broadband usage and the average number of outpatient ED visits per 1,000 long-stay resident days (Figure 2).
By leveraging virtual care modalities to connect with clinical providers, SNFs may be able to reduce the necessity of sending their residents to the local ED. But our findings assume that SNFs operating in well-connected markets are more likely to leverage telehealth services than SNFs that are less connected. We need more robust research on this topic.
As we celebrate Telehealth Awareness Week, we must recognize that telehealth in the nursing home industry is here to stay. I welcome our newest “friend” and look forward to learning how to best use it in the delivery of care. How about you?
Steven Littlehale is a gerontological clinical nurse specialist and chief innovation officer at Zimmet Healthcare Services Group.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.




