
The Center for Medicare & Medicaid Services’ first goal for developing an alternative payment system to replace the current prospective payment system (PPS) structure is to create a model that compensates skilled nursing facilities accurately based on the complexity of the beneficiaries they serve and the resources necessary in caring for those beneficiaries.
With the shift from volume in RUGs IV to a goal of value and patient characteristics in RCS-I, rehab providers should ask themselves:
o Do we know where our patients will fall?
o Do our therapists have a keen understanding of MDS sections C-Cognitive Patterns, G-Functional Status, K-Swallowing and Nutritional Status, and I-Active Diagnoses that will identify their case mix categories?
o Are our therapists actively engaged in MDS data collection aside from Section O?
To understand why therapist will need to improve their knowledge of the clinical components of the MDS, let’s look at some examples.
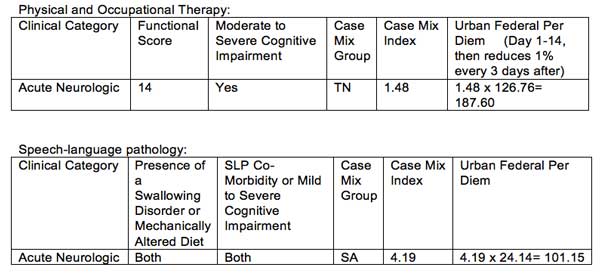
Mr. Adams is a new admission to your skilled nursing facility. He is admitted following a new onset of RCVA. Secondary to new acute onset of stroke, he meets the criteria for acute neurologic for physical and occupational therapy and speech-language pathology; analysis of MDS reveals:
o Section G: Functional Status indicates he requires extensive assist for transfers (+5) and toileting (+3) and limited assist (+6) for eating for a total functional score of 14
o Cognitive Functional Scale reveals a moderate to severe cognitive impairment
o Section K: Swallowing and Nutritional Status indicates presence of a swallowing disorder and presence of mechanically altered diet
o Section I: Active Diagnoses reveals SLP-related Comorbidities of apraxia and aphasia
Physical and Occupational Therapy:
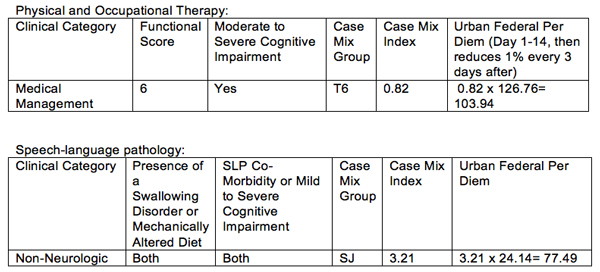
Now, let’s consider an individual patient with significant complexities who is admitted following an acute-care stay and will fall into a medical management classification.
Ms. Jones is admitted to your facility with significant medical comorbidities including diagnoses of COPD and diabetes. During her acute-care stay, she suffered respiratory failure and was subsequently intubated and admitted to your facility with a tracheostomy.
Prior to her acute-care stay, she was living in an assisted living facility with a goal to return to her prior living environment. Activities of daily living are profoundly impaired at admission. Under the RCS-I increased considerations for Ms. Jones, complexities will be accounted within the non-therapy ancillary component.
o Section G: Functional Status indicates she is total dependence for transfers (+2), toileting (+2), and eating (+2) for a total functional score of 6.
o Cognitive Functional Scale reveals a moderate to severe cognitive impairment
o Section K: Swallowing and Nutritional Status indicates presence of a swallowing disorder and presence of mechanically altered diet
o Section I: Active Diagnoses reveals SLP-related comorbidities of tracheostomy and dysphagia.
When comparing Mr. Adams’ and Ms. Jones’ case studies, I am sure you are asking yourself:
Why is the per diem significantly reduced for an individual with the level of impairments we see in a tracheostomy patient, especially considering her goals and prior level of function?
To answer this question, we must understand the foundational differences in RUGs IV and RCS-I, which include unique and distinct components for Nursing and Non-Therapy Ancillary (NTA).
Ms. Jones’ diagnoses of COPD, tracheostomy and diabetes will result in an NTA score of 6 for an NTA group of NC and NTA Case Mix of 2.02. When we factor in the Urban per diem of $76.12 and adjustment factor of 3 for days 1-3, we result in additional NTA reimbursement of $461.29 for the first three days of the stay and $153.76 for the following days within the stay.
So where will your residents fall?
Pull your teams together, have discussions on your internal processes for data collection and accuracy within the MDS, and do not forget to have your voice heard. The comment period for RCS-I has been extended from June 26, 2017, to August 25, 2017.
Renee Kinder, MS, CCC-SLP, RAC-CT, is Director of Clinical Education for Encore Rehabilitation and also serves as the Gerontology Professional Development Manager for the American Speech Language Hearing Association.




