
Mornings are always hectic regardless of the healthcare facility — getting patients up, dressed, a visit to the bathroom, maybe morning meds and fasting blood draws — all before breakfast and the daily activities and/or therapies commence. But now there is mounting evidence that blood does not need to be drawn prior to eating! Such medical conclusions may change the early morning paradigm and how patients are managed.
Traditionally, morning blood draws were required for accurate blood glucose and lipid panel results which helped diagnose metabolic syndrome, diabetes and cardiac risk. Metabolic syndrome is a constellation of conditions that place patients at high risk for coronary artery disease. These include 1) type 2 diabetes, 2) obesity, 3) high blood pressure, 4) elevated cholesterol and triglycerides (and high LDL (bad) cholesterol and low HDL (good) cholesterol) and 5) elevated insulin levels.[i]
 Traditional testing has always held that to get baseline values of blood glucose and lipids the patient had to have fasted for at least 8 hours (some suggest 12 hours) prior to the blood draw.
Traditional testing has always held that to get baseline values of blood glucose and lipids the patient had to have fasted for at least 8 hours (some suggest 12 hours) prior to the blood draw.
Glucose Testing Blood glucose levels were historically used to both diagnose and monitor patients with diabetes. It was a snapshot of the glucose circulating in the blood at a moment in time. Eating most foods would spike the blood sugar and not provide a baseline level that could be compared to previous results. Blood glucose is also used to provide a basic metabolic index that can be translated into a cardiac risk indicator.
Many elderly patients residing in long-term care facilities suffer from some form of metabolic syndrome, diabetes or have other maladies that require the monitoring of glucose. However, studies now show that Hemoglobin A1c is a more useful baseline predictor of disease state than the fasting glucose level.[ii]
In fact, many national and international health societies have updated their guidelines for disease diagnosis and management of patients using Hemoglobin A1c values. Hemoglobin A1c provides an average blood sugar level over the last 120 days — the lifespan of a red blood cell which carries both glycosylated and non-glycosylated hemoglobin. The percent of glycosylated hemoglobin is an indirect measurement of the average amount of blood glucose that is circulating. These historical test results provide a better indication of blood sugar control than the fluctuating plasma blood glucose levels.
Lipid and Cholesterol Testing Lipid panels measure cholesterol, triglycerides, HDL (good) and LDL (bad) cholesterol components. Most at-risk patients are clinically managed by the LDL test result.[iii] Until recently, LDL was a calculated value of total cholesterol minus the HDL minus 1/5 of total triglycerides.
Eating any amount of fat can skew the cholesterol baseline results and affect the calculated LDL value. But new technologies now allow for direct measurement of LDL and thus any non-fasting lipid values do not play a role in the final result.[iv],[v] A recent study analyzed cholesterol test results from more than 200,000 patients who had eaten anywhere between less than one hour to more than 16 hours before the blood draw. The study concluded that both total cholesterol and HDL varied by less than 2%, while LDL varied by no more than 10%.[vi] These findings allow for both calculated and direct LDL to be measured from non-fasted patients with little effect on their clinical results. Eliminating the fasting requirement before lipid panel tests would be more convenient for patients and for labs, which often get slammed for blood draws in the morning when most fasting patients come in, researchers said. “There are logistic challenges when you’re going to get a fasting sample on everybody,” said Dr. J. Michael Gaziano, who wrote a commentary accompanying the new study.[vii]
Blood Pooling Additionally, morning blood draws from bedridden patients can lead to artifacts in testing results. A patient that has had little activity overnight can succumb to a phenomenon often referred to as blood pooling or hemoconcentration.[viii] That is blood drawn from the arm is not at equilibrium with the rest of the body and can lower blood counts—most alarming is a low hematocrit or hemoglobin level. This can lead a medical director to conclude that the patient requires a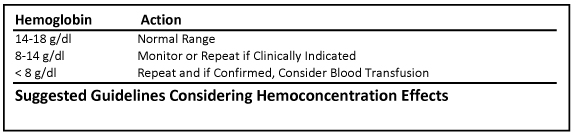 blood transfusion, and if it is a LTC patient, they may be transported to a local hospital, only to be retested and the hematocrit or hemoglobin level is not nearly as low as previously indicated.
blood transfusion, and if it is a LTC patient, they may be transported to a local hospital, only to be retested and the hematocrit or hemoglobin level is not nearly as low as previously indicated.
The process of getting the patient to the hospital has re-equilibrated the blood components and they are more normal and often less alarming, not requiring any intervention. Of course such a transport is not only a concern to the patient and their family members, but represents a considerable expense to the facility or other payer. Furthermore, the laboratory that performed the early morning blood draw is questioned about the quality of the testing result — unfairly so, based on the postural state of the patient.
Such low hematocrit or hemoglobin results, resulting from hemoconcentration, complicate the setting of a threshold for clinical intervention and perhaps a blood transfusion. New evidence from studying 19 different studies, representing over 6,000 patients, concluded that hemoglobin thresholds greater than 7-8 gm/dl triggered unnecessary transfusions without adverse associations of mortality, cardiac morbidity, functional recovery or length of hospital stay.[ix]
The bottom line is that a facility with a patient who has a low hemoglobin result might be advised to retest the patient following some activities that help equilibrate the blood components, prior to transporting the patient to an ER and potentially transfusing a patient unnecessarily. The study suggests that panic values for clinical intervention might be best set at levels of less than 8 gms/dl hemoglobin without adverse patient affects.[x]
Since hospital readmissions are now being tracked and have potential financial penalties associated with them, such guidelines are important for appropriate clinical management of the patient in today’s diminishing reimbursement environment.
Furthermore, more and more long-term care facilities are regulating how early patients can be drawn citing patient abuse concerns, thus narrowing the window of opportunity to draw a patient’s blood. The advantage of drawing patients without regard to meal schedules will allow for a more level workload on both nursing and phlebotomy staff without affecting the clinical results. Such a practice would also help prevent hemoconcentration effects.
In conclusion, these studies all conclude early morning fasting blood draws are becoming less necessary for most traditional clinical laboratory test results—and would allow for one less disruption to a patient early in the morning.
William DePond, M.D., is the Chief Medical Officer and Gary Milburn, Ph.D., is the Chief Technical Officer of MEDLAB, the largest laboratory service provider to LTC facilities in the US.
[i] Metabolic syndrome. National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/health/dci/Diseases/ms/ms_all.html. Accessed Aug. 15, 2011
[ii] International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334
[iii] Castelli WP, Garrison RJ, Wilson PW, et al. Incidence of coronary heart disease and lipoprotein levels: the Framingham study. JAMA 1986; 256: 2835-8.
[iv] Bachorik PS, Ross JW. National Cholesterol Education Program recommendations for measurements of low-density lipoprotein cholesterol: executive summary. National Cholesterol Education Program Working Group on Lipoprotein Measurements. Clin Chem 1995; 41:1414-20.
[v] Nauck M, Warnick GR, Rifai N. Methods of measurement of LDL-cholesterol: a critical assessment of direct measurement by homogenous assays versus calculation. Clin Chem 2002; 48: 236-254.
[vi] Sidhu D,, Naugler C, Fasting Time and Lipid Levels in a Community-Based Population: A Cross-sectional Study. Arch Intern Med. 2012 Nov 12:1-4. doi: 10.1001/archinternmed.2012.3708. [Epub ahead of print]
[vii] Gaziano, J. M., Should We Fast Before We Measure Our Lipids? Arch Intern Med. 2012;172(22):1705-1706.
[viii] Narayanan S., The preanalytic phase. An important component of laboratory medicine. Am J Clin Pathol. 2000 Mar;113(3):429-52.
[ix] Carson, J. L., et al., Outcomes Using Lower vs Higher Hemoglobin Thresholds for Red Blood Cell Transfusion. JAMA, 309:1 83-84. (2013)
[x] Froom, P., et al., Effect of Urgent Clinical Notification of Low Hemoglobin Values, Clin. Chemistry 47:1 63-66. (2001)





