
As agents of innovative health care for the future, our role is clear in paving the path of collaborative efforts within the patient care continuum. Transitional Care Management (TCM) is certainly not a new concept, but as it evolves the interventions are defined from many different perspectives and approaches. In general, care transitions refer to the movement of patients from one health care practitioner to another. TCM not only promotes the necessary links between the health care providers, but promotes the primary concept of endorsing collaboration and early identification of the patient’s risk factors. All of these elements are built into a plan that will prevent adverse outcomes during the transition of care from one level to the next. The TCM model aligns our focus on goals of care and comprehensive planning throughout the health continuum in prevention of readmissions and other unfavorable outcomes.
The Medicare Payment Advisory Commission (MEDPAC) presents costs associated with 30-day hospital readmissions as an estimated $15 billion annually in Medicare spending. The churning of these patients in and out of hospitals comes at a high price to the healthcare system in the form of adverse events, patient dissatisfaction and cost. Of particular threat are patients with complex needs including the vulnerable populations; during transitions throughout the continuum of care these patients are at risk for medical errors, lack of responsiveness to critical labs, or other overlooked symptom indicators. In addition, many other life-threatening elements go unnoted and fall through the cracks during the transition from hospital to sub-acute or long term care. It is anticipated that the prevalence of disjointed care will increase as health care providers continue the move to single practice settings where we no longer have primary providers synchronizing the patient care needs. Taking an aggressive proactive approach is needed to prevent the challenges that face the health care fluctuations anticipated for our vulnerable populations at present and in the near future.
How is the transitional care model relevant in terms of supporting the movement of our elderly population in the long term care (LTC) setting? It is imperative that we elevate our understanding of preparedness by obtaining all critical information as patients are admitted since this population is very likely to be at a much higher risk during the transition phase. Also, establishing the patient’s base line (lab values and other physical findings) with risk factors, immediate intervention needs and treatment that was provided prior to discharge is vital. Our efforts need to emphasize a care management model that supports efficiency across the continuum of care, see figure 1.
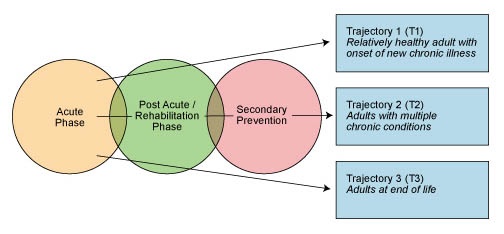
Figure 1: Efficiency Across Episodes of Care
The primary elements of the well-known Coleman Care Transitional Interventions that are relevant in the LTC population are simply stated as medication management, patient-centered health, provider collaboration and proactive risk assessments. In a nutshell, the process is straight forward and the steps are not complicated. The course prescribed in the Coleman Model involves all care providers enacting robust risk assessments, medication reconciliation practices, shared electronic medical records (EMR), meaningful provider discharge documentation and adherence to practice standards of care. All of these elements are required to promote successful transition of the patient from one level of care to the next.
Operative transitional care coordination among hospitals, skilled nursing facilities, lab providers, physicians, home care, hospices and other providers can successfully minimize patient risk and prevent re-hospitalizations. Most of these occurrences are preventable when the team is engaged in this proactive approach. However, effective transitional care doesn’t use one standardized approach to care, but is driven by a unique patient specific plan of care. The core components of transitional care explicit to the long term care population include:
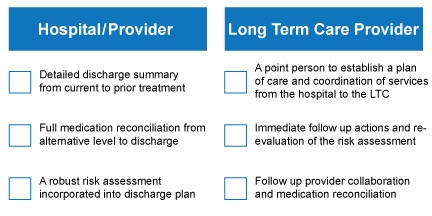
Figure 2: Core Components of Transitional Care
The Affordable Care Act (ACA), the Medicare program effective January 2013, was established to pay doctors for care coordination services when transferring patients to skilled nursing facilities. According to a new coverage policy detailed in the final Medicare physician fee schedule published Nov. 1, the new service was one of a myriad of Medicare payment changes finalized in the annual regulation announcing program rates for the next year.
Based on the work of MEDPAC, the Affordable Care Act (ACA) focused initially on three conditions: heart attack (AMI), heart failure and pneumonia. In 2015, the policy will incorporate COPD, CABG, PTCA and other vascular conditions as identified by MEDPAC in its June 2007 report. Identifying the patient population at risk is not difficult. The key is to assess the needs of this vulnerable population and present quick interventions based on the established medical protocols. As our aging population grows, the overall legislative and technological environment will continue to evolve, changing the way that we manage our patients. Moving forward, practices that engage patients, caregivers and providers in a collaborative approach will be the best option to ensure quality of life at all levels. The questions that we need to ask ourselves as health care providers is once the patient’s risk is identified, are we responding in a preventive mode of treatment and are we adjusting our care models to meet this new evolution of preemptive patient care?
Debra Jacobs, RN, CRRN, CCM, B.S., M.S.N. is the vice president of clinical services at MEDLAB.
REFERENCES
1. Darwin, B & Parrish, M. California Healthcare Foundation: Navigating Care Transitions in California: Two Models for Change. Sept 2008. Accessed 2/21/13 http://www.chcf.org/publications/2008/09/navigating-care-transitions-in-california-two-models-for-change.
2. Naylor, M. & Sochalski, J. Scaling Up: Bringing the Transitional Care Model into the Mainstream. The Common Wealth Fund, Nov, 2010. Accessed 2/20/13. www.wapatientsafety.org/downloads/TCM_Forefront.pdf
3. American Geriatrics Society (AGS) Position Statement: Improving the Quality of Transitional Care for the Persons with Complex Care Needs. March/April, 2007; Accessed 2/20/13 www.caretransitions.org/…/Improving%20the%20quality%20-%20J.
4. Kannan,S. The CHCF Care Transition Projects: Final Progress Report and Meeting Summary. March, 2009. Accessed 3/1/13. www.chcf.org/resources/download.aspx?id=%7B9E8C3A8A…
5. Figel, C. National Health Service Corps: Medicare finalizes physician pay for new care coordination benefit. Accessed 2/22/13 http://www.ama-assn.org/amednews/2012/11/12/gvl11112.htm
6. Center for Medicare Advocacy Inc.: Accessed 2/21/13 http://www.medicareadvocacy.org/2012/05/02/medicare-hospital-readmissions



