
Recently I traveled to Portland, OR, for a cousin’s wedding of my cousin. Everything was beautiful, but as we drove through the state, everyone noticed the heavy smoke. Forest fires are raging through Oregon and Washington, and many find it difficult to breathe outdoors.
 That’s one of the reasons I was fascinated by data from Care at Hand, whose client base includes Spokane-based Aging & Long Term Care of Eastern Washington. ALTCEW is one of 13 Area Agencies on Aging that contract with the state department of health to provide in-home care and community-based services. When he talked to Care at Hand about the fires, CEO and co-founder Andrey Ostrovsky, M.D., said it was a good chance to change quality indicators to avoid hospitalizations for certain patients.
That’s one of the reasons I was fascinated by data from Care at Hand, whose client base includes Spokane-based Aging & Long Term Care of Eastern Washington. ALTCEW is one of 13 Area Agencies on Aging that contract with the state department of health to provide in-home care and community-based services. When he talked to Care at Hand about the fires, CEO and co-founder Andrey Ostrovsky, M.D., said it was a good chance to change quality indicators to avoid hospitalizations for certain patients.
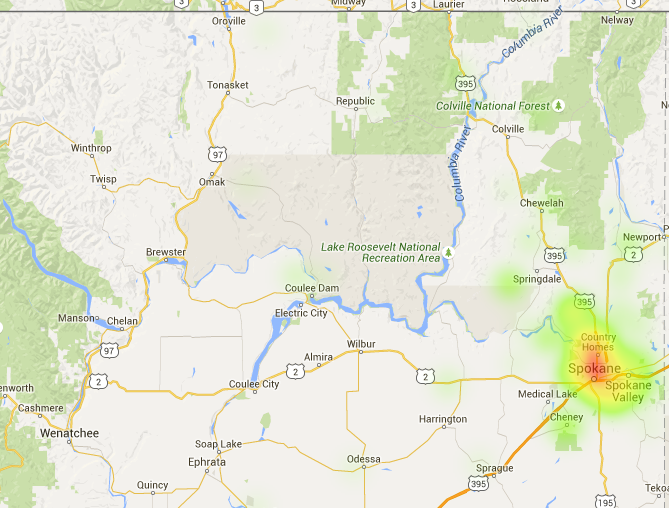
Care at Hand was able to highlight patients who were at risk, such as those with respiratory illness, those who have COPD or had pneumonia recently, those using oxygen, and smokers. There were 55 patients flagged as being predisposed to having problems — i.e. landing in a hospital emergency room or, down the road, a long-term care facility. As I’ve said before, long-term care tends to ignore home- or community-based service technology and data mining, but the era of bundled payments, partnerships and accountable care mean it’s time to pay attention.
ALTCEW said the report was helpful in identifying and prioritizing patients and creating a workflow plan for coaches to follow up. The agency focused on tracking those patients down and giving guidance, direction and planning.
Of course, technology gets healthcare services only so far.
The forest fire report “opened up a can of worms,” Ostrovsky told me. In disaster situations such as this, senior citizens, especially those with existing health problems, often pack their bags and leave. The guess is they start with family members, but they could eventually end up in an ER or nursing home far away from their home-base care teams.
In addition, it’s not uncommon for this population to not return phone calls or, in some cases, answer the door.
“There’s a good chunk where we have no idea where they are,” Ostrovsky said. “They are poor, elderly, frail, with glaucoma and aren’t logging into Facebook. It’s a big concern.”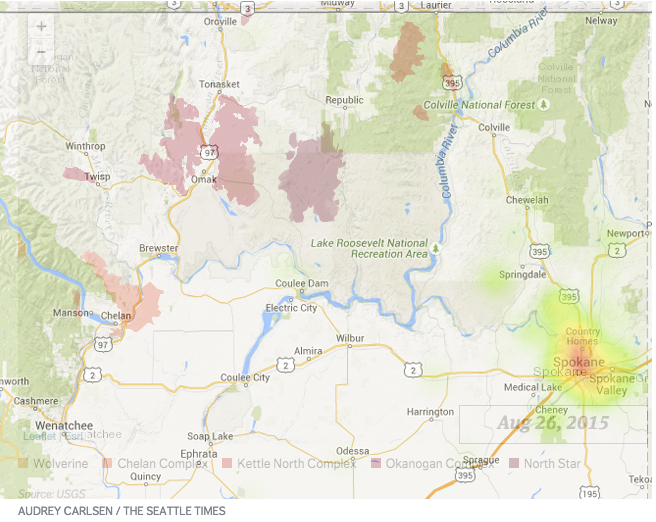
But there are multiple silver linings. One, ALTCEW was able to prioritize who its highest risk clients were. Two, it was relatively easy to ascertain the group was far away from the fire. Three, it is a reminder technology can’t solve everything. Short of having everyone over age 65 microchipped, like you might a family pet, providers and agencies have to work with seniors on the importance of checking in.
“If the processes aren’t robust, if you can’t engage the consumer, how are you going to track?” Ostrovsky said. Ultimately, data is only as good as a provider’s ability to figure out what to do with it.
Elizabeth’s Etiquette Tip for the Week:
On the note of flying, the most common bad behavior I have observed recently is rudeness getting off or on the plane. I promise you that pushing that child out of the way will not make the plane take off faster. Also, stop glaring at the woman stepping onto the plane with a baby. She’s having a tougher trip than you are.
Elizabeth Newman is Senior Editor at McKnight’s Long-Term Care News. Follow her @TigerELN.



